Health
End-of-life care
|
Improving care at the end-of-life is a growing global public health priority and an important aspect of people-centred health policies. In recent years, awareness about end-of-life care (EOLC) has climbed on the policy agenda and has led to discussions around the development and appropriateness of palliative care, life-sustaining care and social services in virtually all OECD countries. The COVID-19 pandemic has also exposed many pre-existing issues and raised new challenges regarding EOLC services and policies to improve people’s well-being at the end-of-life. The OECD began working on EOLC in 2020, aiming to review how health systems in OECD countries are addressing EOLC and to identify useful practices and evidence-based strategies. The final report “Time for better care at the end of life” has been released on 7 February 2023. |
|
LAUNCH OF THE OECD REPORT “TIME FOR BETTER CARE AT THE END OF LIFE”
 |
The OECD report Time for better care at the end of life has been released on 7 February 2023. Speakers and participants included national experts, academic experts, representatives of the private sector, workforce representatives and representatives of civil society. It aimed to highlight the growing priority of improving end-of-life care as well as discuss the way forward in terms of policies in the areas of workforce, quality, funding and governance. |
WHY IS END-OF-LIFE CARE IMPORTANT
People at all ages can benefit from receiving a high-quality EOLC. However, as populations are ageing, the need for EOLC is likely to increase. This is all the more important as more people are ageing with chronic and disabling conditions, and the largest increase has occurred among the oldest – people 80 years of age and older. In this scenario, the number of people dying of diseases that would benefit from palliative care and EOLC is forecasted to increase from 6.3 million in 2017 to 9.7 million in 2050.
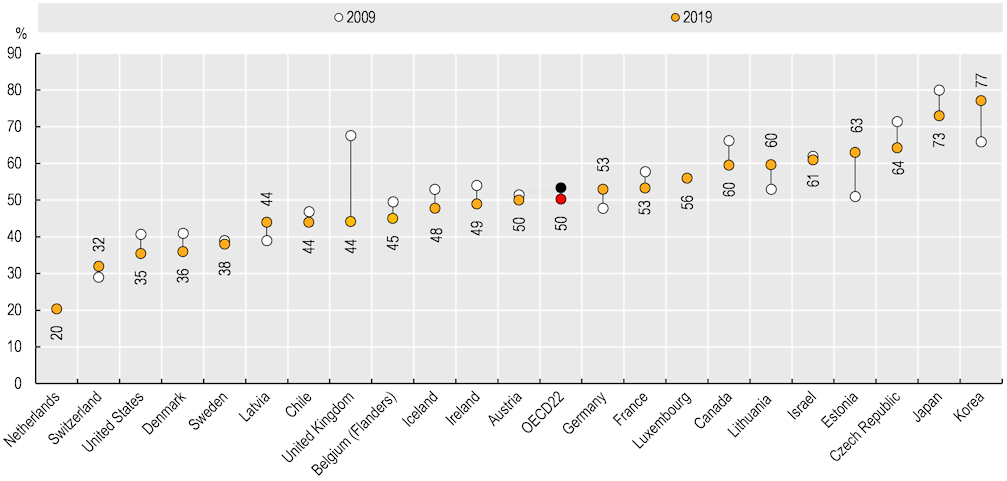
EOLC needs to be more people-centred. The place of care at the end-of-life is important for patients and their families, while also for governments and other stakeholders when it comes to planning and policy-making. Initial analysis of data in some OECD countries shows that hospitals are still the predominant place of death, accounting for 50% of deaths on average and for over 70% in some countries.
Trends in hospital death rates, 2009-19 (or nearest year)
Note: Data for the Czech Republic include hospices and nursing homes classified as health establishments.
Sources: National sources and OECD EOLC-HCQO pilot data collection, 2021.
Access the data.
FURTHER READING
- Read the chapter dedicated to Ageing and Long-term Care in Health at a Glance 2023: OECD Indicators
- Access our latest data from OECD Health Statistics in the dataset Long-term care resources and utilisation
- Find out more about our work on Ageing and Long-term Care
- Health Statistics
Related Documents