Health
Integrated Care
|
Across OECD countries, ageing populations and increasing numbers of people with chronic diseases shift the focus of healthcare services away from acute care addressing longer episodes of healthcare needs. Almost two in three people aged over 65 years live with chronic conditions. This has fuelled the debate on the need for integrated delivery systems capable of addressing continuous, coordinated, and high quality care delivery throughout people’s lifetime. In recent decades, OECD countries have introduced integrated care initiatives aimed at ensuring individuals receive the right care, in the right place, at the right time, but existing organisational and financing structures appear to hamper their success. |
|
JUST RELEASED - International comparisons of the quality and outcomes of integrated care
 |
International comparisons of the quality and outcomes of integrated care: Findings of the OECD pilot on stroke and chronic heart failure Across OECD countries, two in three people aged over 65 years live with at least one chronic condition often requiring multiple interactions with different providers, making them more susceptible to poor and fragmented care. This has prompted calls for making health systems more people-centred, capable of delivering high-quality integrated care. Despite promising, mostly local-level, experiences, systems remain fragmented, focused on acute care and unsuitable to solve complex needs. Moreover, assessing and comparing the benefits of integrated care remains difficult given the lack of technically sound, policy-relevant indicators. This report presents the results of the first OECD pilot of a new generation of indicators to support international benchmarking of quality of integrated care. Lessons from the pilot call for further work on: (1) expanding work on indicator development; (2) performing policy analysis to understand cross-country variations on governance models and health financing; (3) upscaling data linkage; and (4) measuring care fragmentation.
|
The report provides five key messages:
1. When reviewing national best practices, countries collect a growing volume of data but the lack of systematic data linkage at patient level undermines the value of the data to inform performance measurement for integrated care.
2. The 2020-2021 OECD pilot data on Integrated Care covered 15 countries and developed a new generation of indicators on mortality, readmissions and prescribed medicines for post-discharge care in stroke and congestive heart failure using linked data at patient level over a six-year period.
3. The pilot showed data collection is feasible, but linkage remains a challenge - 15 countries submitted data on mortality and readmissions but only four countries (Czech Republic, Denmark, Finland and Sweden) provided post-discharge medicine prescription data.
4. Data analysis suggests that OECD average masks large cross-country variations in outcomes within one year after discharge while trend analysis within countries shows improvements in outcomes. More analysis with multiple indicators and increased data linkages are required to measure integrated care.
5. To improve the international comparability of future data collections the OECD will refine the indicators and integrate into routine data collections the indicators on mortality and readmissions for post-discharge care in ischaemic stroke and congestive heart failure.
The report proposes further work on (1) expanding indicator development for future data collections in three possible directions:
- Go broad - by expanding work to other patient cohorts, conditions and diseases
- Go deep - by considering longer care trajectories and further linkages along the health system and between health and social care
- Go towards other dimensions - by measuring other performance dimensions such as access, utilisation and cost, or care fragmentation
and (2) performing policy analysis to explore cross-country variations by mapping integrated care policies and reviewing system-level care integration innovations and policies in the areas of governance and organisation of care delivery, information systems, and health financing.
WHAT IS INTEGRATED CAre ?
The recent pandemic has only amplified the need for various parts of the health systems to work together to deliver seamless care. While the care of patients often focuses on acute care in hospitals, patients’ experiences and outcomes of care depend on how care is provided across a pathway of services. These begin before access to acute care, and extend well beyond a patient’s stay in hospital. As patterns of morbidity shift, the integration of hospital services with out-of-hospital care will be critical.
Ongoing OECD work in this area aims to:
- develop quality and outcome indicators to support cross-country comparison in the effective delivery of integrated care across healthcare settings; and
- identify policies to improve incentives, care models and governance arrangements aimed to tackle care coordination problems in health systems.
A new generation of indicators has been piloted and published in Health at a Glance 2023: OECD Indicators, see indicator on Integrated Care, to kick-start international benchmarking of quality measurement of integrated care. The pilot consisted of a set of three types of indicators providing insight into the quality of integration between hospital and community care one year after hospitalisation for people suffering from stroke and congestive heart failure:
- All-cause and disease-specific hospital readmissions;
- All-cause mortality after hospital discharge; and,
- Prescription of appropriate medication for secondary care prevention after hospital discharge.
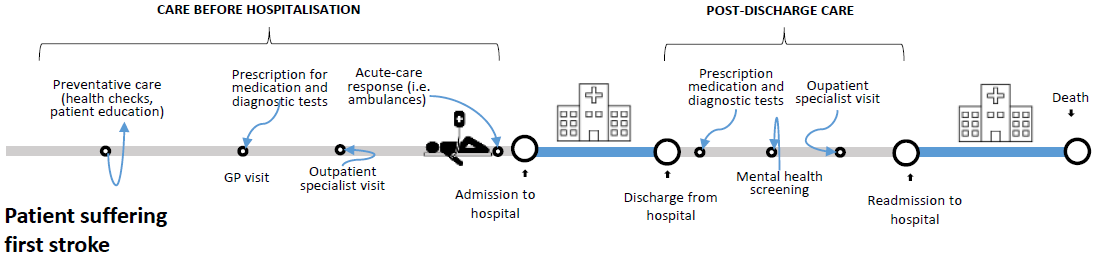
These indicators take a patient care pathway perspective by using “country-wide” electronic health records systems and data linkage at patient level across existing data sets to follow key events on a journey across the system for a person (as illustrated in the infographics below).
A technical report with detailed data analysis and next steps for future OECD work was published in May 2022: see International comparisons of the quality and outcomes of integrated care, Barrenho et al., OECD Health Working Paper No. 142.
Example of a patient's journey: key events within the health system experienced by a first-time stroke patient
Source: Authors, adapted from Sund and Hakkinen in (Cylus J, Papanicolas I and Smith PC, 2016).
KEY DATA
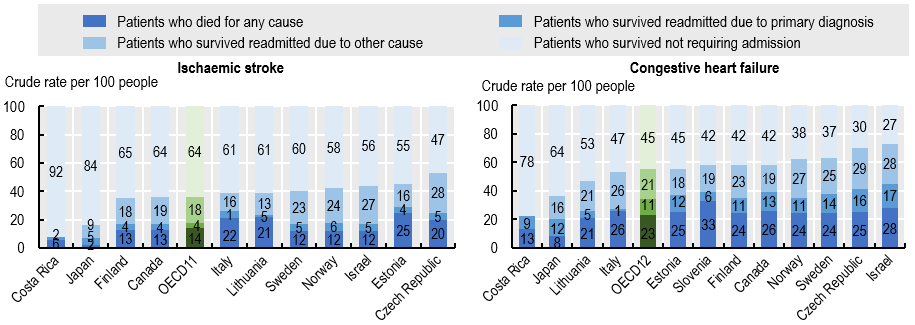
The graphs below show the mortality and readmissions outcomes across OECD countries in the year after discharge following ischaemic stroke or CHF in 2018. For patients who suffered an ischaemic stroke, on average, 64% survived and did not return to acute care, 22% survived and were readmitted to hospital (4% for stroke-related and 18% for other reasons) and 14% died in the following year. For CHF patients, on average, 45% who survived did not return to acute care, while 32% survived but were readmitted for CHF related or other causes and 23% died in the following year.
For patients who suffered a stroke and were discharged, 1-year mortality ranged from 2% in Japan to 25% in Estonia. For CHF patients, 1-year mortality varied from 8% in Japan to 33% in Slovenia. 1-year readmissions of stroke patients surviving one year or more ranged from 1% in Lithuania to 6% in Norway for stroke-related reasons, and from 0% in Costa Rica to 28% in the Czech Republic for non-stroke causes. For patients with CHF surviving one year or more, readmission rates varied from 1% in Italy to 17% in Israel for CHF-related causes and from 0% in Costa Rica to 29% in the Czech Republic for other causes.
Patient outcomes within one year of discharge after ischaemic stroke and congestive heart failure, 2018
Access the data behind the graphs.
Source: OECD HCQO Pilot Data Collection on Integrated Care 2021, in Health at a Glance 2021: OECD Indicators.
FURTHER READING
- Read about Integrated Care in Health at a Glance 2023: OECD Indicators
- Read our new series of country reviews of health information systems: Towards an Integrated Health Information System in Korea (May 2022) and Towards an Integrated Health Information System in the Netherlands (February 2022)
- Find out more about our work on Healthcare Quality and Outcomes Indicators
- Learn about the Patient-Reported Indicator Surveys (PaRIS)
- Read our report Health for the People, by the People: Building People-centred Health Systems
- Learn about the project Towards person-centered integrated care in Italy
- Browse all our Health Publications
CONTACT US
- Ms Eliana Barrenho: eliana.barrenho@oecd.org
- Generic contact: hcqo.contact@oecd.org

Follow us on Twitter @OECD_Social
Related Documents